Before traveling into the cells of our body under the guidance of Jean-Marc Sabatier and to fully understand the pitfalls of current vaccines against SARS-CoV-2 and their necessary evolution to new generations, it is important to know that there are three types of antibodies
1- “Neutralizing” antibodies that will fight and neutralize the virus. These are the ones most familiar to the general public. Their production is desired during a vaccination;
2- “Neutral” antibodies that will recognize the Spike protein of SARS-CoV-2, involved in the infection of cells, but will not be protective;
3- “Facilitating” antibodies which, contrary to “neutralizing” antibodies, will promote the infection of cells by the virus (these antibodies are found during the vaccination of cats against the FIP virus, as well as during the vaccination against SARS-CoV-2 at the origin of Covid-19 in humans). It is these antibodies that should not be produced during vaccination.
However, all current vaccines based on the SARS-CoV-2 Spike protein contain these three types of antibodies. Hence the difficulties that we see after vaccination of some patients. Hence also the worrying vaccine strategy of the 3ᵉ or 4ᵉ dose recommended, including in France, for patients with co-morbidities (obesity, diabetes, hypertension, etc.). Jean-Marc Sabatier explains why.

In a previous interview, you demonstrated the strong similarities between the cat virus, known as FIP (feline infectious peritonitis) virus, and the SARS-CoV-2 virus that causes Covid-19. Yet vaccine trials in cats have been counterproductive. Why has this been the case?
We have seen that the coronavirus of FIP (feline infectious peritonitis) in cats has strong similarities with the SARS-CoV-2 coronavirus that causes Covid-19 in humans. We have also seen that not only do vaccination trials of cats with an avirulent strain of FIP not protect vaccinated cats but, on the contrary, promote infection of cats subsequently exposed to a virulent strain of FIP virus.
These data show the existence (in this case) of a phenomenon called “ADE” (antibody-dependent enhancement). In this mechanism, “facilitating” antibodies are present. These antibodies bind to the FIP virus and facilitate the infection of cells by the virus. Indeed, phagocytic cells (monocytes, macrophages, dendritic cells…) have a receptor (called FcgRIIa) capable of recognizing antibodies attached to the viral particle, which allows the infection of these cells by internalization of the virus-antibody complex.
ADE in respiratory infections is included in a broader category called ERD (“enhancement of respiratory diseases”) which also includes non-antibody based mechanisms (such as cytokine storms and cell-mediated immunopathology) that promote the infectious process and deleterious effects of the virus.
Recently, an abnormally high proportion of people vaccinated against SARS-CoV-2 have been shown to have more severe forms of Covid-19 than in viral infection of unvaccinated people.
By analogy with the FIP virus in cats, it seems conceivable that the “ADE” phenomenon (or “ERD” in general) may be found in vaccination against SARS-CoV-2.
What should be done?
The objective is to produce a vaccine Spike protein that is unable to bind to the ACE2 receptor in order to avoid the potential direct deleterious effects of the Spike protein and to avoid the “ADE” (or even “ERD”) phenomenon.
The “challenge” is therefore to preserve (as much as possible) the “key” elements of recognition of the Spike protein by the immune system, i.e. the regions of the Spike protein that will be recognized by the immune system of the host (the vaccinee) and that will induce a protective neutralizing immunity.
More precisely, it is a question of preserving the protective B and T epitopes (specific regions of the Spike protein recognized by the immune system). B epitopes induce antibody production by activated B cells, while T epitopes are recognized by T cells (cytotoxic lymphocytes) responsible for fighting and destroying virus-infected cells.
Therefore, “facilitating” B epitopes that promote SARS-CoV-2 infection of cells should be removed (whenever possible).
What about current vaccines?
The idea is to render the vaccine Spike protein inert by modifying it so that it is unable to bind to its ACE2 receptor and overactivate the renin-angiotensin system (RAS). This is not the case with current vaccines, either mRNA or attenuated viral vector (adenovirus) vaccines.
In other words, vaccines can produce the same effects as SARS-CoV-2 and be shown to lead to Covid-19 disease.
These vaccine proteins have been shown to have the potential to bind to the ACE2 receptor and overactivate the RAS that causes Covid-19 diseases. A healthy individual could thus develop Covid-19 diseases following vaccination.
Worrying. How can we correct this?
By modifying the vaccine Spike protein so that it becomes unable to bind to its target (the ACE2 receptor) and trigger potential Covid-19 diseases. In addition, this Spike protein would ideally need to be modified to remove the regions that contain the “facilitating” B epitopes.
Is this technically possible?
It is feasible by identifying the regions of the Spike protein that are responsible for the production of the “facilitating” antibodies and removing them from the final structure of the vaccine Spike protein. This requires prior work to identify the “facilitating” B epitopes.
Another approach is to produce synthetic vaccines based on peptides (fragments of the Spike protein) that mimic the protective B and T epitopes of the Spike protein.
Why didn’t the big laboratories do it?
Because the laboratories went for the simplest (I guess it was already complicated) in creating their vaccines. The Spike protein is a large molecule that has two parts: an outer S1 subunit (which allows binding to the ACE2 receptor) and an S2 subunit, which allows fusion of the virus and target cell membranes. Current vaccines are based on a modified Spike protein from which they have removed the S2 subunit involved in the membrane fusion process.
Here, the external S1 subunit should also be modified by removing the “facilitating” regions that will promote the infection of cells by the virus.
So, theoretically, new vaccines can be made quickly?
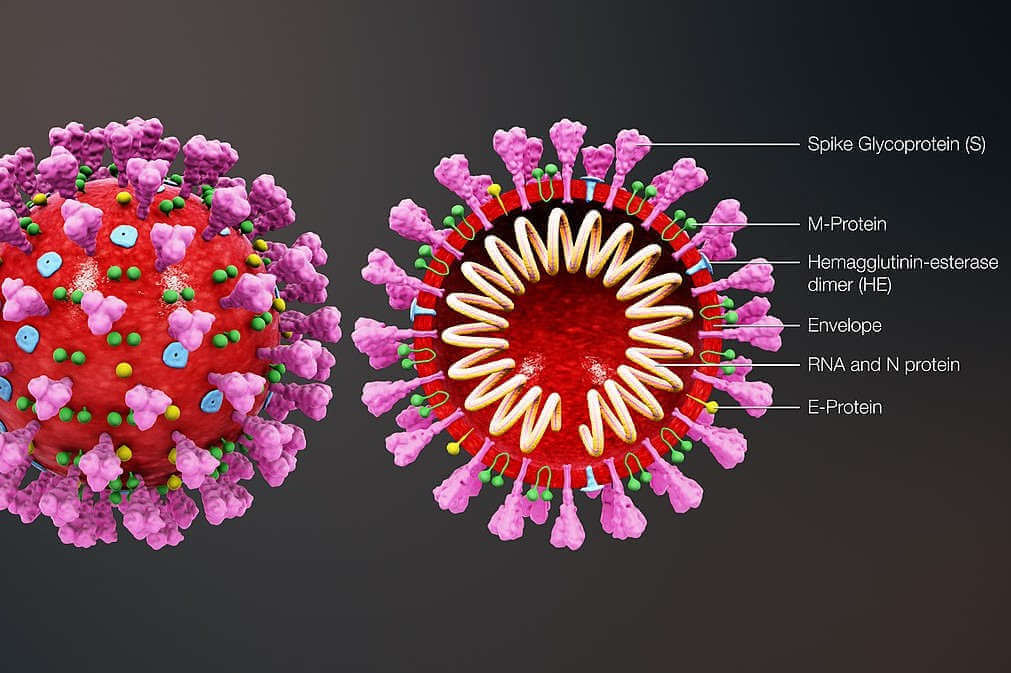
It is also possible to produce synthetic vaccines based on molecules (peptides) that mimic B (“neutralizing”) and T (protective) epitopes of the Spike protein. Peptides derived from other SARS-CoV-2 viral antigens (these antigens are the nucleocapsid protein N, the envelope protein E, the viral membrane protein M, and the fusion glycoprotein hemagglutinin esterase, which are essential for coronavirus infectivity) can be added.
In other words, the majority of vaccines are based on the Spike protein: it is possible to add one or more other viral antigens in order to increase the effectiveness of the vaccines.
For example, the Chinese vaccines Sinopharm (Eponym) and Coronavac (Sinovac) are based on inactivated SARS-CoV-2, which means that in theory they could provide superior protection to the others, as they have all the viral antigens. However, chemical inactivation of the virus causes changes in these antigens that can lead to a less effective protective immune response. This chemical inactivation of the virus leads (among other things) to changes in the three-dimensional structure of these viral antigens.
So vaccination does not fully protect?
The natural immunity conferred by infection with SARS-CoV-2 and its variants appears to be much greater than that conferred by vaccination. This natural immunity is based on the stimulation of the infected person’s immune system against all viral antigens.
Based on current data, it appears that the natural immunity conferred by SARS-CoV-2 is approximately ten times greater than that conferred by vaccination against the Spike protein.
What will the next generation of vaccines look like?
This suggests “new” avenues for a future generation of effective vaccines that are free of side effects.
In this new generation of vaccines, it will be necessary – in my opinion – to produce a Spike protein modified so that it is no longer able to bind to the ACE2 receptor of the target cells.
- By preventing overactivation of the RAS, we should prevent the onset of potential Covid-19 diseases;
- By deleting the “facilitating” B epitope of the Spike protein, a more effective humoral immune response (antibodies) should be obtained;
- By adding one or more viral antigens to this vaccine composition, one could increase the protective potential of the vaccines.
Such a strategy is also valid for the development of an effective vaccine against FIP virus in cats.
Given this, do you support the injection of a 3rd or even 4th dose of vaccine, starting at the beginning of the school year, for patients with co-morbidities?
If the “ADE” (or even “ERD”) phenomenon exists with current vaccination, it is likely that these vaccine boosters (3ᵉ and 4ᵉ doses) would increase the proportion of “facilitating” antibodies, leading to an effect potentially opposite to that sought. The cure would then be worse than the disease.
*Jean-Marc Sabatier, Research Director at the CNRS and Doctor in Cell Biology and Microbiology, affiliated with the Institute of NeuroPhysiopathology (INP), at the University of Aix-Marseille. Editor-in-Chief of the international scientific journals: “Coronaviruses” and “Infectious Disorders – Drug Targets” (DR)