Three scientists demonstrate here in a masterly way that the coronavirus could be transmitted essentially by large sputters to the glass and to the plate during meals. They also explain how to protect oneself from it. Cross interview.

Stéphane Odasso, why, in your opinion, is the spit a high risk during a meal taken opposite?
SO: We know that SARS-CoV-2 can be present in spittle, droplets and aerosols that are exhaled when talking, coughing, sneezing, and even singing. The postillion is millimetre-sized, while the droplets and aerosols are microscopic in size, around a generally accepted separation value of 5 microns, with the aerosols being smaller than 5 microns (1). Posticles are ejected from the mouth, from saliva, which may be loaded with virus (2): thus the risk of infection from posticles is strongly related to the salivary viral load. To simplify, the higher the viral load, the greater the risk of exceeding the infection threshold proposed by some authors, which is between 100 and 1000 virions. Thanks to our new online simulator, we can evaluate the theoretical risk according to the viral load present in saliva: for a 1 mm diameter spit and an average viral load of 3.3 106 virus copies per ml, we obtain approximately 1700 copies present in a single spit, which is much higher than the theoretical infectivity threshold. It is therefore quite understandable that a single spit sent on a plate and put in the mouth represents a notorious danger for a receiving host sitting at a table. With a patient with a high viral load, (3.3 108 copies/ml), we get about 170 000 copies of virus, at least 200 times above the theoretical threshold!
Are simulations available to understand this risk at the table?
SO: A Japanese study by the University of Riken/Kobe used the Fugaku supercomputer (the fastest in the world), to visualize the risk of droplet transmission between 4 people sitting at the table. During a meal, the transmitter can sputter by talking next to and in front of it, into the plate and beyond to the center of the table, where the dishes, cutlery, etc. are located.
Considering the trajectory and the fate of the spittle, once ejected through the mouth, the spittle being heavier, they are sensitive to gravity and do not travel more than 1 or 2 meters away, while the aerosols much less rich in virions, they remain suspended in the air with longer times. The simulation video illustrates this clear difference in ballistic behavior between the droplets falling into glasses or plates (yellow droplets very rich in virions) and the aerosols (blue particles with very little virion content).
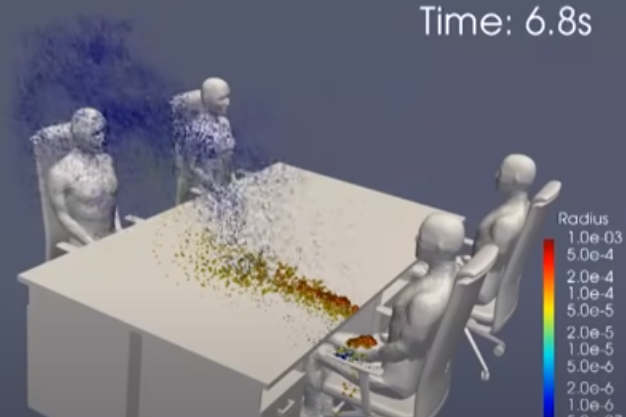
It is therefore understandable why table neighbors opposite or next to the transmitter have a significant risk of contracting covid-19 during a meal in a restaurant.
Jean-Michel Wendling, can you give us some examples where shared meals or drinks could be considered as the source of contamination?
JMW: Yes of course, there are many: for example, a well-documented cluster occurred in February during a dinner in the municipality of Capannori in a 70m² room (Lucca), Italy. Three guests coming from the Milanese region in the 14 days prior to the dinner were symptomatic at this meal (coughing). Out of 49 participants, 26 people developed one or more symptoms. Three subjects were hospitalized and treated and one died. The guests were placed around 5 tables and mingled by changing places during the evening (3) .
Many clusters with shared meals were described in the press. For example, in August, 51 out of 72 gendarmes of the Mobile Gendarmerie squadron of Tarbes tested positive several days after their departure from French Polynesia. On July 31, we note the organization of an evening at the restaurant “piment rouge” and on Monday, August 3, organization of a farewell drink which could be at the origin of the contagion to COVID-19 according to observers. *
Numerous weddings, anniversaries and other family events** where people eat and drink together have led to clusters between July and October in France and abroad. There is no shortage of examples and they have not been the subject of scientific publications but of observations and monitoring documented by the ARS.
And what about in a professional setting, could the meal also be involved?
JMW: Indeed, we have the example of the site of Germany’s largest slaughtering and cutting group Tönnies in Rheda-Wiedenbrück (North Rhine-Westphalia), where 1,553 of the 6,000 employees tested positive for coronavirus. A video *** (54 sec) shows very clearly a crowded canteen, huge tables with workers in work gowns, without the slightest physical distancing. In addition, the company was hiring seconded workers (mostly from Eastern Europe), contract workers, subject to catastrophic housing conditions according to journalists.
More recently and locally, in a dermatology practice where the practitioner works all day long with an FFP2 mask, due to the proximity to the patients for certain treatments, an evening was organized with a pharmacist colleague who had rhinitis (previously falsely negatively tested). At the end of this common evening, outside of the professional setting, all 5 friends found themselves infected in the days that followed.
And these are only 2 examples among a multitude!
The students were also, at the beginning of the school year, very concerned?
JMW: Indeed, at the beginning of the academic year, the students who organized integration evenings (meals with shared drinks) were very numerous and were at the origin of clusters motivating the closure of many schools or university campuses (ECAM Strasbourg-Europe, EM Strasbourg and Lyon, Ecole de commerce Nantes, Faculté de Médecine de Nantes, Ecole Centrale de Lyon, Sciences Po Paris, ENSAS…). The President of the University of Cergy notes that the contaminations are linked to “everything around the university”, i.e. “bars, restaurants, places of socialization which are vectors of transmission of the virus” and Frédérique Vidal, the Minister of Higher Education and Research states that the strong circulation of the virus was outside the educational framework: “clusters are not clusters by promotion, they are clusters by groups of friends”.
Pascal Mensah, do epidemiological studies shed light on risk?
PM: The Center for Disease Control and Prevention (CDC) in the United States points to the role of restaurants and bars. Restaurants and bars would be particularly susceptible to Covid-19 contamination. This is logical, since it is impossible to eat or drink while wearing a mask. However, few studies have so far tried to classify public places according to their risk of being infected by the new coronavirus.
The Centers for Disease Control and Prevention (CDC) in the United States administered questionnaires to 314 people who came for testing in July at 11 U.S. hospitals, half of whom were positive case-patients (n=154) and half of whom were negative controls (n=160). The purpose of the questions was to track where patients were seen in the 2 weeks prior to the onset of their symptoms. Had they gone shopping? Did they take public transportation? Were they in an enclosed area with more than 10 people? Did they go to the office, gym, hairdresser, bar, restaurant?
Case-patients were twice as likely to have eaten in a restaurant (including outdoor patio and seating) in the 2 weeks prior to the onset of illness as control participants (aOR = 2.4). Limiting the analysis to participants with no known close contact with someone with a confirmed VIDOC-19, case-patients were even more likely to report eating out (aOR = 2.8) than control participants. The over-risk was almost 4 times higher for bars and coffee shops in the absence of close contact with a confirmed VIDOC-19 (aOR = 3.9)(4).
Edifying! More examples?
JMW: a very interesting study involving a total of 27 cases followed 347 identified close contacts. The infection rates among contacts “after eating a common meal” 10.6% (17/160) were higher than the parameter “sharing a room/bed” 10.0% (20/201). Working” contacts were identified as associated with 5.3% of secondary cases (5/94). Contacts “with neighbors” (0/30), “medical services” (0/18) and “sharing vehicles with patients” (0/17) were never involved as having generated secondary cases (5).
Using contact data from 1038 confirmed cases of SARS-CoV-2 between January 23 and April 28, 2020 in Hong Kong, researchers identified and characterized all local infection groups. They identified 51 clusters (n = 309 cases) and estimated that 19% of the cases were responsible for 80% of all local transmissions. The authors observed that transmission occurred most often within households (92/169, 54.4%), followed by bars, weddings, religious sites and restaurants (56/169, 33.1%). These social encounter situations were associated with younger people. (6)
Jean-Michel Wendling, could the catering staff pass on the Sars-Cov 2 to the customers?
JMW: We know that on the Princess Diamond ship that was heavily hit by the Covid19 , meals were regularly served via buffets with service personnel for drinks and dishes. The study of this mega-cluster shows that 16/20 of the crew who were sick were working in the catering (n=14) or beverage service (n=2). We can hypothesize that the large contingent of sick catering staff may have accelerated the spread of the virus among the cruise passenger population via food (meal preparation, order delivery).
Another indicative example on an important cluster discovered during a wedding on Lake Annecy. Out of 93 people on board a boat (88 guests, 2 catering staff and 3 crew members), 21 were contaminated. One employee of the wedding caterer was identified as positive. But by the time he found out, he had already worked for another event in the Ain, where 40 people were present. Two guests tested positive on the second event. This transmission is compatible with the fact that the caterer’s employee was probably responsible for the contamination of the guests on the second (cascade) service, and even during the first service of the wedding on Lake Annecy.
Stéphane Odasso, can the “aerosol” transmission identified as causal be questioned in certain reference studies in your opinion?
SO: Absolutely, so in the study of the restaurant in Wuhan (7), on which hundreds of scientists have relied, there is much to criticize: three independent close families were infected. We can note that no PCR test was performed on the staff, neither in the dining room nor in the kitchen. The possibility of transmission by formites has not been explored by surface sampling, even though it is strongly suspected that this mode of contamination may have occurred during a meal.
Furthermore, none of the T18 or T17 tables were contaminated as if a physical boundary was present at this location, which is surprising to say the least. Finally, physically, the aeraulic flow at the level of table A (supposed index patient) then B, and finally back to table C by possible aerosols, leads to an important aerodilution, making contamination unlikely on particles of the order of micron emitted by speech.
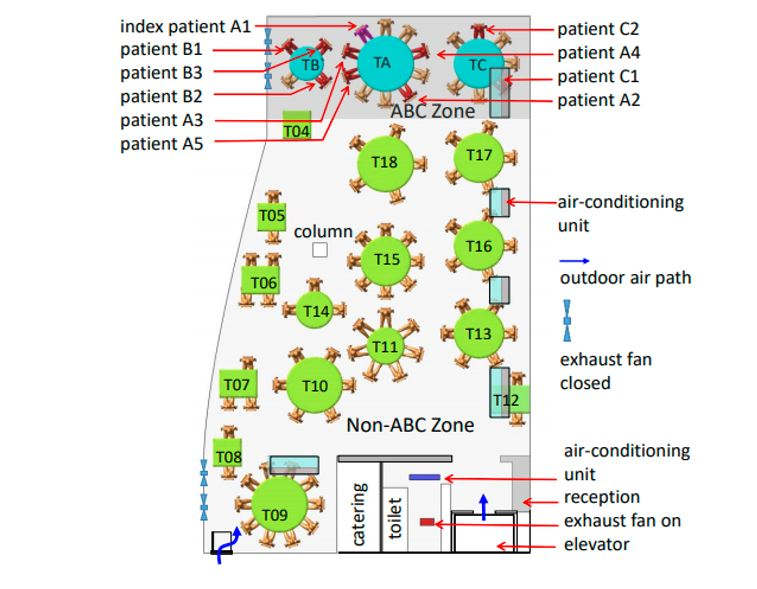
JMW: This configuration is also compatible with a sick leader for example (a series of tables assigned to a single individual), which could be the common denominator of transmission, or who by getting his hands dirty while clearing TA contaminated the plates with TB and CT.
Another often cited example is the 122-member choir in Skagit, Washington, D.C., which met several times for practice every Tuesday night until March 10. Of the 61 people who attended on March 10 during which one person was known to be symptomatic, 53 cases were identified, of which 33 were confirmed and 20 probable. Three of the 53 people who became ill were hospitalized (5.7%) and two died (3.7%). It can be noted that the authors mention snacks (oranges and cookies) and that fomites such as holding hands or stacking chairs at the end of the practice may have been involved, which many scientists and the press have obscured by seeing only the risk of transmission by aerosols (8).
Finally, another example where the authors went very quickly to their conclusion: an observational study dated January 19, 2020 where 128 people took two buses for a round trip to attend a cult. The people who went to this cult in the bus with the patient with VIDOC-19 had a higher risk of infection than the people who took the other bus. The authors conclude that the aerial spread of SARS-CoV-2 appears to have contributed to the high attack rate in the bus exposed via the aerosol-borne air conditioning system. No surface samples were taken from the bus, especially from the handrails, whereas viral RNA was found on a very large number of contaminated surfaces in public transport. Moreover, the notion of meal was not taken into account on the possible common times before and after this event. Finally, the notion of snacks on the bus was not further explored (9).
We can see in all these examples that the scientific approach has been oriented by the a priori hypothesis of aerosol transmission, on this hypothesis alone without exploring the others…
Dirty hands
Pascal Mensah, apart from the spit, the dirty hands, as we have mentioned, do they play a possible role during the meal?
PM: The coronavirus present in the gastrointestinal tract and in the stools at high concentrations (10e8/gr) suggests that it can be present on the hands if they are not properly washed when leaving the toilets, hence the hygiene precautions to be taken, in particular, for the kitchen staff and before going to the table, this seems essential to us! Please note that if you do not wash your hands before a meal as a customer, you can contaminate the cutlery, the bread basket, the bread by helping yourself with your hands, or get infected by sucking your fingers or rubbing your eyes.
On the food side, despite the discovery of Sars-Cov 2 on frozen Brazilian chicken, salmon cutting boards and shrimp packaging, the risk of foodborne transmission has been assessed as low by the World Health Organization (WHO), the HCSP and other international health (such as the US CDC or FDA) and food safety authorities, as well as the Australian and New Zealand governments. These contaminations are undoubtedly the result of contamination from workers in the food chain: cooking food destroys the germ.
Preference should be given to packaged foods. Fruits can be washed with soapy water and rinsed (recommendations of Pr Timothy Newsome, professor-researcher in virology – infectiology – vaccinology at the University of Sydney). Other foods can be cooked or boiled. Wang et al. indicate that heat and humidity can reduce the transmission of CoV-2-SARS (10). Fresh produce that can, and put in the refrigerator, should be cooked.
Innovative prevention measures
What concrete prevention measures can we then propose for a hypothetical reopening of restaurants during the Christmas period?
Appropriate measures could be generalized and tested in restaurants, school and university canteens and refectories such as :
- menus accessible by QR code,
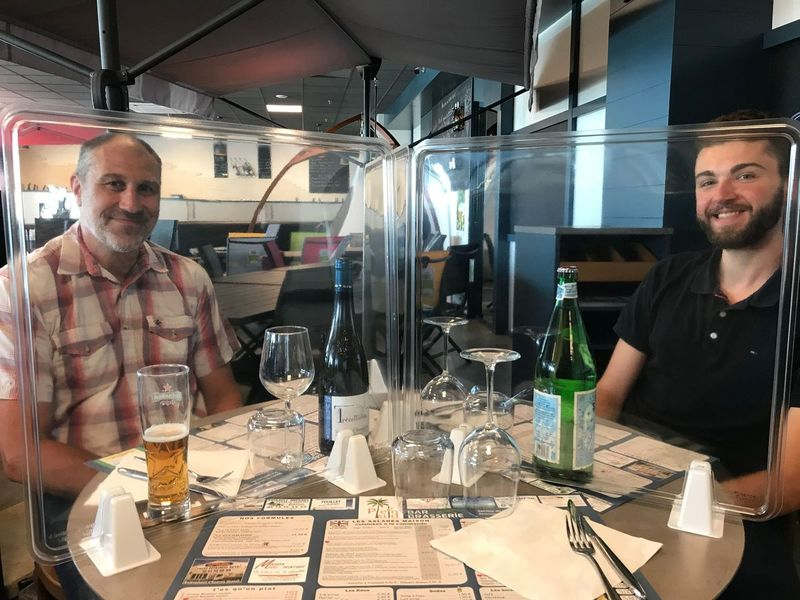
- Plexiglas screens on buffets and tables separating guests (only guests from different families), already installed in many high school canteens (Molière Paris), middle schools (Camille Claudel, Villeneuve), company canteens (Jean Bal Thermoformage) and some restaurants (Plein Sud, Longué-Jumelles),
- the disinfection of upright plates (UVled system for example) before being served, (experimentation in progress)
sanitary facilities equipped with non-contact sensor taps - the use of self-disinfecting coatings that destroy Sars-Cov2 on surfaces touched by the hands (handles, handrails, work surfaces with more than 1000 companies equipped with French technology including Corsair, CAF des Alpes Maritimes, University of Montpellier, Tesalys…)
- the provision of hydroalcoholic gel at each table to allow very frequent hand washing,

The food service sector is very much looking for practical solutions and the chef of the starred gourmet restaurant “La Maison des Têtes” in Colmar, Eric Girardin, after having implemented all the barrier measures very early on, is already at the forefront of health safety in France by implementing some of these solutions in a test experiment. We all need to regain serenity and a more normal life, in safety optimized according to Eric Girardin! (Photo)



Références
- Asadi, S., Cappa, C.D., Barreda, S. et al. Efficacy of masks and face coverings in controlling outward aerosol particle emission from expiratory activities. 24 sept 2020 Sci Rep 10, 15665 (2020). https://doi.org/10.1038/s41598-020-72798-7
- Wang W, Chen S, Liu I, Chen Y, Chen H, Yang C, et al. Detection of SARS-associated Coronavirus in Throat Wash and Saliva in Early Diagnosis. Emerg Infect Dis. 2004;10(7):1213-1219. https://dx.doi.org/10.3201/eid1007.031113
- Orsucci G., Rocchi R., Menconi A., Salvoni F. A., Studio retrospettivo su un focolaio di CoViD-19 sviluppatosi a febbraio durante una cena nel comune di Capannori (Lucca), Recenti Prog Med 2020; 111: 602-605. doi 1701/3453.34420
- Kiva A. Fisher et al. Community and Close Contact Exposures Associated with COVID-19 Among Symptomatic Adults ≥18 Years in 11 Outpatient Health Care Facilities — United States, July 2020 Weekly / September 11, 2020 / 69(36);1258–1264
- Zhonghua Liu Xing Bing Xue Za Zhi Analysis on transmission chain of a cluster epidemic of COVID-19, Nanchang 2020 Sep 10;41(9):1420-1423. doi: 10.3760/cma.j.cn112338-20200313-00334.
- Adam DC, Wu P, Wong JY, Lau EHY, Tsang TK, Cauchemez S, Leung GM, Cowling BJ. Clustering and superspreading potential of SARS-CoV-2 infections in Hong Kon Nat Med. 2020 Sep 17. doi: 10.1038/s41591-020-1092-0. Epub ahead of print. PMID: 32943787.
- Yuguo Li Evidence for probable aerosol transmission of SARS-CoV-2 in a poorly ventilated restaurant doi: https://doi.org/10.1101/2020.04.16.20067728
- Lea Hamner High SARS-CoV-2 Attack Rate Following Exposure at a Choir Practice — Skagit County, Washington, March 2020 Weekly / May 15, 2020 / 69(19);606–610 https://www.cdc.gov/mmwr/volumes/69/wr/mm6919e6.htm?s_cid=mm6919e6_w
- Shen Y, Li C, Dong H, et al. Community Outbreak Investigation of SARS-CoV-2 Transmission Among Bus Riders in Eastern China. JAMA Intern Med. Published online September 01, 2020. doi:10.1001/jamainternmed.2020.5225
- Wang J, Tang K, Feng K, Lv W. High Temperature and High Humidity Reduce the Transmission of COVID-19. Available at SSRN 3551767. 2020; https://doi.org/10.2139/ssrn.355176
Vidéos
* Soirée au Piment Rouge pour les gendarmes de Tarbes
** Mariages et anniversaires :
- Plus de 100 contamination après un mariage à Orléans
- Le mariage se transforme en cauchemar : 7 morts et plus de 170 personnes contaminées
*** Covid-19 : 730 employés d’un abattoir contaminés ( 54ème seconde du reportage)
Recommandations
Précision
Les trois scientifiques interviewés déclarent ne pas avoir de liens d’intérêt avec les entreprises citées proposant des solutions innovantes de protection contre les virus.
