The story of a fundamental French discovery, that of Pr Jean-Marc Sabatier, which could revolutionize the understanding and treatment of this decidedly mysterious disease. Interview.

Jean-Marc Sabatier reveals this fundamental discovery he made with virologists from Wuhan (China) in March 2020 (published in April): “COVID-19 like diseases appear when a ubiquitous hormonal/physiological system in the human body, called the renin-angiotensin system SRA, malfunctions, even in the absence of the SARS-CoV-2 virus”. Explanations.
The “real” culprit?
-Jean-Michel Wendling: What would be, according to you, the “real” culprit for the manifestations of COVID-19?
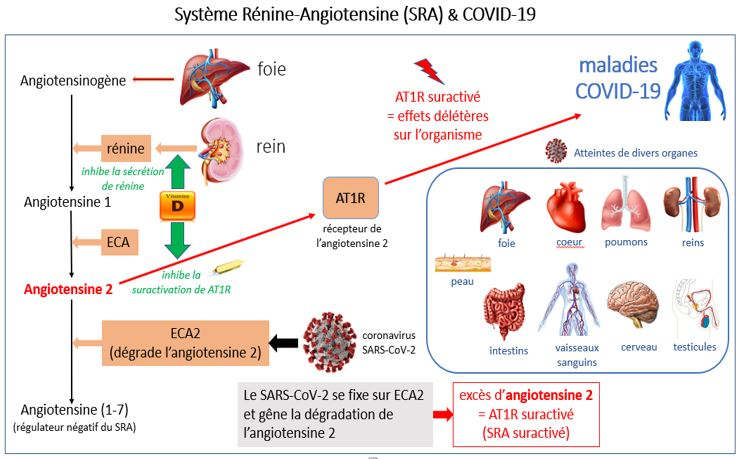
Jean-Marc Sabatier: The “renin-angiotensin system” (RAS) is the “real” one responsible for COVID-19, and SARS-CoV-2 is the oil that is put on the fire. Indeed, COVID-19-like diseases can occur even in the absence of a virus, when the RAS has gone too far and is working too hard.
As early as March 2020, I had spotted the extraordinary analogies between the consequences of an SARS-CoV-2 infection and the consequences of a malfunction of this “key” system. These analogies were reported in a scientific publication (accepted in April) (1) that my collaborators also co-authored, including Prof. Zhijian Cao and Prof. Yingliang Wu, directors of the virology laboratory in Wuhan (China). When infected with the SARS-CoV-2 virus, it binds to the ECA2 (angiotensin-2 converting enzyme) receptor of the target cells, which normally has the function of degrading angiotensin-2. This binding of CoV-2-SARS to the ECA2 receptor thus prevents normal degradation of angiotensin-2, resulting in an increase in its concentration and overactivation of its cellular target, the AT1R receptor.
-What is the AT1R receptor?
The overactivated AT1R receptor is highly deleterious to the human body through the very harmful storm of released cytokines (TNF-alpha, interferon-gamma, interleukin-6, interleukin-1-beta, etc.). These mediators are responsible for the evolution of COVID-19 to severe (even fatal) forms.
The renin-angiotensin system (RAS) (1,2) is a “key” hormonal/physiological system found throughout the body and particularly in: lungs, kidneys, intestines, heart, brain, testes, blood vessels, as well as cells of the “innate” immune system (circulating monocytes, macrophages, dendritic/antigen presenting cells, Natural Killer cells, etc.). The RAS controls “innate” immunity (non-specific “immediate” response to pathogens) and the intestinal microbiota.
Virus-free COVID-19s?
JMW: What would be the “COVID-19-like” diseases that would be caused by RAS without the presence of the virus?
JMS: The SRA is responsible for COVID-19-like diseases via an overactivation of its “deleterious” AT1R (1) receptor. This activated receptor mainly induces vasoconstriction/hypertension, inflammation, oxidative stress, nitric oxide depletion, organ hypertrophy and fibrosis. This “deleterious” effect results in the potential appearance of symptoms and diseases such as : high blood pressure, atherosclerosis, hypertrophy (heart, blood vessels), fibrosis (heart, lungs, kidneys, liver), heart failure, kidney and lung damage (asthma), anosmia (loss of smell), agueusia (loss of taste), neurological disorders / memory disorders, diarrhea, intestinal and vascular inflammation, lipid metabolism dysfunction, obesity and action on glucose metabolism (diabetes), thrombosis / coagulopathy, skin and testicular lesions (1,2,3,4). In addition, it appears that “deregulated” RAS may be closely linked to the onset of neurological disorders, cancers, and other autoimmune diseases (multiple sclerosis, rheumatoid arthritis, etc.), through its actions on the central nervous system, cell proliferation and adhesion, and “innate” immunity.
In-depth knowledge of the physiological repercussions of an RAS “runaway” finally allows us to describe, understand, and anticipate all the “COVID-19” diseases associated with an SARS-CoV-2 infection.
Vitamin D at the center of all hopes
-JMW: Could this renin-angiotensin system (RAS), in its deleterious runaway, be hindered by drugs already on the market or candidate drugs?
JMS: Yes, the diseases (and symptoms) of COVID-19 could be thwarted or even treated by molecules capable of “slowing down” over-activation of the RAS. Several known molecules are “brakes” on overactivated RAS: vitamin D(1,5,6 ), dexamethasone, a corticoid widely used in advanced forms, but also certain angiotensin degradation products (angiotensin 1-7, angiotensin 1-9, alamandin, angiotensin A, and angiotensin IV active respectively on the MasR, AT2R, MRGD, ECA2, and AT4R cellular receptors) (7,8).
Among these molecules, vitamin D is very important. It can be easily administered and has a low cost. It is indispensable in people with deficiency (cholecalciferol or vitamin D3). Such supplementation is necessary, particularly in this period of a viral pandemic (5), and takes into account the vitamin D deficiency/deficiency of the majority of the population.
In France, according to the 2006-2007 National Nutrition and Health Study, the prevalence of vitamin D deficiency shows that 79% of men and 81% of women had a serum calcidiol concentration (the form of vitamin D hydroxylated in the blood by the liver) of less than 75 nmol/l (the optimal threshold). For 36% of men and 49% of women it was below 50 nmol/l (moderate deficiency) and below 25 nmol/l (severe deficiency) for 4% of men and 6% of women.
In 2019, the GRIO (Groupe de Recherche et d’Information sur les Ostéoporoses) will offer patients at risk, after measuring the initial level, a regimen of 50,000 IU of vitamin D (cholecalciferol) per week for 4 to 8 weeks depending on the deficiency. This period of rapid “recharging” could then be followed by a long-term treatment of 50,000 IU/month, the effectiveness of which will be verified after 3 to 6 months. This additional dosage of calcidiol is necessary because of the very large inter-individual variability in the rise in calcidiol after a given dose of vitamin D3, with some patients raising their calcidiol levels only slightly, while in others the increase is very large. Vitamin D intoxication is rare but can be caused by daily supplementation at too high doses. According to the National Academy of Medicine, vitamin D intoxication is not associated with calcidiol concentrations below 250 nmol/l, which leaves an extremely wide margin between the optimal threshold (75 nmol/l) and the risk of overdose.
Vitamin D thus slows down the overactivated RAS by inhibiting renin secretion by the kidneys. In addition, it regulates the expression of 291 genes (nearly 1000 genes in high supplementation), including genes for “innate” and “adaptive/acquired” immunity. Its action on the human body is very beneficial and allows a good functioning of the immune system to fight various pathogens (it induces the production of specific anti-microbial compounds, including cathelicidin and defensins). Vitamin D helps prevent progression to severe forms of COVID-19 during CoV-2 SARS infection, while reducing the likelihood of becoming infected and the duration of viral carriage (6).
The Academy of Medicine recommended early on (press release of May 22) vitamin D supplementation, which is still insufficiently known to date.
Useful anti-hypertensive drugs
Very recently, ACE inhibitors and AT1R blockers/antagonists used for the treatment of hypertension have also been shown to be effective “brakes” on RAS (1).
In a multi-center retrospective study published on October 30, 2020, of 2190 adult patients admitted for laboratory-confirmed COVID-19 at three participating centers, clinical course, dyspnea and fatigue were significantly improved in patients, particularly those over 65 years of age, who were taking antihypertensive drugs involved in RAS. In addition, clinical outcomes were significantly improved (statistically) in patients taking antihypertensive medications after statistical adjustment for age, gender, baseline blood pressure and co-existing medical conditions (9).
An Italian team showed, consistent with our work, that in 411 hypertensive patients over 68 years of age, ACE inhibitors and AT1R inhibitors/antagonists were associated with lower COVID-19 mortality, after adjustment for 32 variables in the medical history (10).
New” candidate molecules
According to an Indian researcher from the ICMR (National AIDS Research Institute) and also consistent with our findings, MasR agonists have also shown organ protective effects in several animal studies. Nevertheless, these agonists have not been tested in clinical studies. Their evaluation in COVID-19 affected and critically ill patients is urgently recommended by Prof. Ashwini Shete in order to reduce mortality associated with viral infection (8).
-JMW: Is there any specific information you would like to add on RAS in COVID-19?
JMS: Yes, it has been reported that men are statistically more susceptible to CoV-2-SARS than women, with children being less affected than adults. It is interesting to note that the activity of SRA (e.g., ECA2 expression) varies between men and women (this system is carried by the sex chromosome X); it also varies strongly with age from birth to death of an individual (children versus adults).
JMW: This discovery is a great hope for the care of patients.
Interview by Dr. Jean-Michel Wendling, scientific advisor for infodujour.fr
Références
- SARS-CoV-2 & COVID-19: Key-roles of the renin-angiotensin system / Vitamin D impacting drug and vaccine developments. Cao, Z., Wu, Y., Faucon, E., Sabatier, J.M., Infectious Disorders-Drug Targets, 20, 348-349 (2020). Doi: 10.2174/1871526520999200505174704
- ACE2 – From the renin-angiotensin system to gut microbiota and malnutrition. Perlot, T., Penninger, J.M., Microbes and Infection, 15, 866-873 (2013).
- Montelukast drug may improve COVID-19 prognosis: a review of evidence. Barré, J., Sabatier, J.M., Annweiler, C., Frontiers in Pharmacology, 11:1344 (2020). Doi: 10.3389/fphar.2020.01344.
- Neurological, cognitive and behavioral disorders during Covid-19: the nitric oxide track. Annweiler, C., Bourgeais, A., Faucon, E., Cao, Z., Wu, Y., Sabatier, J.M., Journal of American Geriatrics Society, 10.1111/jgs.166671 (2020). Doi: 10.1111/jgs.166671
- Point of view: Should COVID-19 patients be supplemented with vitamin D? Annweiler, C., Cao, Z., Sabatier, J.M., Maturitas, 140, 24-26 (2020). Doi: https://doi.org/10.1016/j.maturitas.2020.06.003
- Vitamin D and survival in COVID-19 patients. A quasi-experimental study. Annweiler, C., Hanotte, B., de l’Eprevier, C.G., Sabatier, J.M., Lafaie, L., Célarier, T. J. Steroid Biochem. Mol. Biol. 204, 105771 (2020). Doi: 10.1016/j.jsbmb.2020.105771
- Counter-regulatory ‘renin-angiotensin’ system-based candidate drugs to treat COVID-19 diseases in SARS-CoV-2-infected patients. Annweiler, C., Cao, Z., Wu, Y., Faucon, E., Mouhat, S., Kovacic, H., Sabatier, J.M., Infectious Disorders-Drug Targets, 20, 407-408 (2020). Doi: 10.2174/1871526520666200518073329
- Urgent need for evaluating agonists of angiotensin-(1-7) /Mas receptor axis for treating patients with COVID-19. Shete, A., International Journal of Infectious Diseases, 96, 348-351 (2020). Doi: 10.1016/j.ijid.2020.05.002
- Antihypertensive drugs are associated with reduced fatal outcomes and improved clinical characteristics in elderly COVID-19 patients. Yan, F., Huang, F., Xu, J., Yang, P., Qin, Y., Lu, J., Zhang, S., Ye, L., Gong, M., Liu, Z., Wei, J., Xie, T., Xu, K.F., Gao, G.F., Wang, F.S., Cai, L., Jiang, C., Cell Discovery, 6(1), 77 (2020). Doi: 10.1038/s41421-020-00221-6
- Exposure to renin-angiotensin system inhibitors is associated with reduced mortality of older hypertensive Covid-19 patients. Gori, M., Berzuini, C., D’Elia, E. et al (pré-publication) medRxiv 2020.12.15.20247999; doi: https://doi.org/10.1101/2020.12.15.20247999

