As for Alzheimer’s disease, Jean-Marc Sabatier establishes for the first time a direct link between Parkinson’s disease and the dysfunctional renin-angiotensin system. Explanations.

By Jean-Marc Sabatier
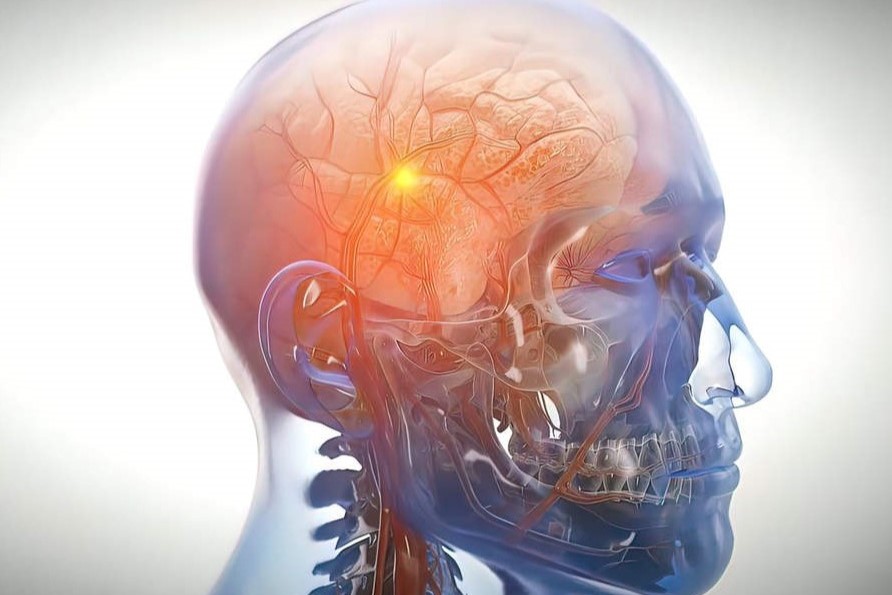
The neurodegenerative disease of Parkinson
Parkinson’s disease affects more than 9 million people worldwide, including more than 200,000 people in France (incidence of 3.2 men out of 1000, and 2 women out of 1000). It is the second most common neurodegenerative disease in France, after Alzheimer’s disease. The disease is chronic and of slow progressive evolution over several years, and is rarely observed before the age of 45, with a prevalence between 85 and 89 years (a genetic origin is found in 5% of cases). It is a neurodegenerative pathology associated with motor symptoms such as tremors at rest (dopamine deficiency induces depolarization of acetylcholine neurons in the striatum), slow movements (bradykinesia), rigidity of the limbs (hypertonia) or stiffness of movements (due to exacerbated tension of the muscles causing cramps and various muscular or tendon pains), and postural imbalance.
400,000 neurons in the substantia nigra
The disease is also characterized by mental, cognitive, sensory (including pain), and sleep disorders. During Parkinson’s disease, the destruction of a specific population of neurons is observed: the dopamine neurons, called dopaminergic neurons. These neurons are involved in the control of movements and are found in the substantia nigra (or locus niger) of the brain. The substantia nigra (subdivided into pars compacta and pars reticulata) is a small nervous structure made up of approximately 400,000 dopaminergic neurons (these neurons are pigmented because they contain neuro-melanin), whose cell bodies transmit extensions into the striatum, which constitutes a large cerebral nucleus.
Dopamine is the neurotransmitter present in large quantities in the pre-synaptic terminals of these neurons, hence their name dopaminergic neurons. They can release dopamine on structures in the striatum called the caudate nucleus and the putamen.
Lesions of the substantia nigra
Thus, the substantia nigra and the striatum are brain structures that are very rich in dopamine (the pars reticulata of the locus niger is made up of GABAergic neurons). In people suffering from Parkinson’s disease (Parkinson’s patients), lesions of the substantia nigra of the brain are observed, corresponding to a progressive disappearance of dopaminergic neurons; this results in a depletion of dopamine in this region of the brain. At a more advanced stage, the dopamine deficiency no longer allows the activation of the striatum, whose dopamine content also decreases significantly. The substantia nigra becomes pale because the number of dopaminergic neurons decreases.
Mysterious aggregates
Within the remaining dopaminergic neurons, inclusions (Lewy bodies) appear which are characteristic of Parkinson’s disease. Lewy bodies are “mysterious” aggregates of proteins in the neuronal cell, made up of neurofilaments (the main structural proteins of neurons) and mostly of alpha-synuclein (a protein involved in the formation of synapses). In Parkinson’s disease, neuronal death – especially of dopaminergic neurons in the early phase of the disease – appears to be linked to the formation of these protein aggregates, as well as to inflammation of the brain tissue involving microglial cells (innate immunity) and T lymphocytes (adaptive/acquired immunity). In Parkinson’s patients, the natural alpha-synuclein protein changes its three-dimensional structure, and acquires an “abnormal” spatial shape favoring the formation of protein aggregates. Moreover, the “abnormal” alpha-synuclein is able to transform “normal” alpha-synuclein into an “abnormal” form. This change in the three-dimensional structure of alpha-synuclein spreads within the same dopaminergic neuron and then is transmitted from neuron to neuron in the nigro-striatal region of the brain responsible for movement coordination.
Certain metals and pesticides promote the disease
The damage (synucleinopathy = presence of Lewy bodies) of Parkinson’s disease is not limited to the dopaminergic neurons of the substantia nigra; it can be observed in the cerebral dopaminergic neurons of the olfactory bulb, the cortico-mesolimbic pathways, and the enteric nervous system (neurons of the intestine). In advanced disease, other neuronal populations associated with neurotransmitters distinct from dopamine (such as serotonin, norepinephrine and acetylcholine) are affected by nerve degeneration and synucleinopathy. In Parkinson’s disease, people remain asymptomatic until 50-70% of the dopamine neurons are destroyed (brain plasticity allows for compensation of this neuronal loss).
It is notable that exposure to certain metals or pesticides favors the onset of Parkinson’s disease, while coffee and/or tobacco consumption seems to be protective. Parkinson’s patients infected with SARS-CoV-2 have a 30% increased risk of dying from Covid-19, including pneumonia.
The renin-angiotensin system (RAS) and its dysregulation (e.g. SARS-CoV-2 and vaccine spike protein)
The SARS-CoV-2 virus causes the overactivation/dysregulation of a physiological system central to the functioning of the human body: the renin-angiotensin system or RAS (also known as the angiotensin-aldosterone system or AAS). The RAS is responsible for renal, pulmonary, and cardiovascular autonomic (automatic) functions; it also controls innate immunity and the various microbial flora (microbiota) of the body. The RAS is ubiquitous in the human body because it is present in the cells of various tissues and organs. The dysfunctional RAS (because it is overactivated) is directly responsible for Covid-19 pathologies via the excess of the hormone angiotensin-2, which releases aldosterone and overactivates the “deleterious” receptor AT1R. Indeed, the AT1R receptor overactivated by excess angiotensin-2 possesses numerous activities that are harmful to the human organism, via the triggering of cellular signaling cascades. The overactivated RAS and AT1R receptor are pro-hypertensive (vasoconstriction of blood vessels), pro-inflammatory (storm of pro-inflammatory cytokines), pro-oxidant (production of deleterious reactive oxygen particles), pro-thrombotic (formation of clots that obstruct blood vessels), pro-angiogenic (growth of blood vessels and tumors) pro-hypoxemic (decreased oxygen loading of red blood cells), pro-hypoxic (impaired oxygen delivery to cells, tissues and organs), pro-fibrosing (organ fibrosis), pro-hypertrophying (cardiac and vascular hypertrophy), and nitric oxide depletion (impaired inflammatory, immune and memory processes).
Overactivated RAS and Parkinson’s disease
Parkinson’s disease has been observed in some people following natural infection with SARS-CoV-2 and/or Covid-19 vaccination. For example, Dr. Pardis Zarifkar (Copenhagen National Hospital, Denmark) reports a 2.6-fold increased risk of developing Parkinson’s disease in the Danish population following SARS-CoV-2 infection (the risk appears to be 3.5-fold higher in the case of Alzheimer’s disease).
Australian researchers (University of Queensland, Australia) have shown that SARS-CoV-2 can cause brain inflammation. The involvement of RAS in neurological diseases has been demonstrated. RAS components can be produced and active within cells (intracrine RAS activity), especially in the central nervous system. As previously described, viral infection with SARS-CoV-2 (or even anti-Covid-19 vaccination) causes RAS dysfunction, via excess angiotensin-2 inducing aldosterone secretion by the adrenal glands, and overactivation of the “deleterious” AT1R receptor responsible for Covid-19 diseases.
Overactivation of the RAS is accompanied by hypertension, a major factor in neurodegenerative disorders and impairment of brain function. RAS inhibitors (e.g. sartans, ACE inhibitors of angiotensin-1 converting enzyme) have been shown to have beneficial effects on neurodegenerative diseases and cognitive dysfunction. Excess angiotensin-2 hormone is thus associated with neurological disorders. Nervous system cells (neurons, oligodendrocytes, astrocytes and microglial cells) have the ACE2 (angiotensin-2 converting enzyme) receptor on their surface which is a target of the SARS-CoV-2 spike protein (or vaccine spike protein). Binding of the spike protein to the ACE2 receptor induces excess angiotensin-2 and overactivation of the pro-inflammatory AT1R receptor: the latter induces a storm of pro-inflammatory cytokines and inflammation, including inflammation of brain tissue via activated M1 microglial cells (innate immunity) and T cells (adaptive/acquired immunity).
Neurovascular uncoupling
The AT1R receptor is also pro-oxidant and stimulates a redox enzyme (NADPH oxidase Nox) responsible for an increase in the number of reactive oxygen particles in the mitochondria (energy centers of cells) inducing mitochondrial dysfunction and programmed neuronal or cell death (by apoptosis). Similar to the formation of intracellular aggregates of tau protein or extracellular amyloid beta protein in Alzheimer’s disease, the accumulation of intracellular protein clusters of neurofilaments and alpha-synuclein (Lewy bodies) in Parkinson’s disease must be due to overactivation of the RAS. It is notable that the pro-hypertensive effect of the overactivated RAS contributes to limit blood flow in the brain, favoring neuro-vascular uncoupling, cerebral hypometabolism and the development of neurological damage.
How to counteract the disorders associated with Parkinson’s disease and resulting from RAS dysfunction?
In Parkinson’s disease, the drugs used are generally dopamine and molecules that allow dopamine synthesis (L-Dopa is a precursor of the neurotransmitter). A strategy of extra-cranial illumination by infrared is even being tested in Grenoble to reactivate dopamine secretion! Other molecules of interest block the monoamine oxidase B (MAO-B) and co-methyltransferase enzymes involved in the degradation of dopamine (e.g. selegiline for the MAO-B enzyme) in order to increase its life span. Supplementation with tyrosine and phenylalanine (two aromatic amino acids) helps dopamine synthesis, as well as micronutrients (copper magnesium, zinc, manganese, vitamins PP, B6 and B9, etc.). The various inhibitors of the RAS are important, including vitamin D through its action as a negative regulator of the RAS (by inhibiting the production of renin) and its protective effects against cognitive dysfunction, neurodegenerative and cerebrovascular disorders. At the level of the RAS, angiotensin-2 is able to bind to the AT1R and AT2R receptors with very different affinities. These RAS receptors are expressed in brain regions related to autonomic, cognitive, and movement control functions. The AT1R and AT2R receptors are found in the pars compacta (“black part” composed of dopaminergic neurons afferent to other brain structures: the caudate nucleus and the putamen belonging to the striatum) of the locus niger, which is responsible for most of the dopamine production. In addition, various elements of the RAS have been identified in dopaminergic neurons, which are the preferred cellular targets in early Parkinson’s disease.
As for Alzheimer’s disease, there is a direct link between the dysfunctional renin-angiotensin system (because overactivated by the viral or vaccine spike protein) and the neurodegenerative disease of Parkinson’s. Obviously, other neurodegenerative diseases are also associated with RAS dysregulation, whether or not they are dependent on host infection with SARS-CoV-2. This is illustrated by the clearly beneficial and protective effects of RAS inhibitors on the incidence and severity of neurological pathologies in humans.
Covid : collection of Jean-Marc Sabatier’s censored articles in English and Spanish